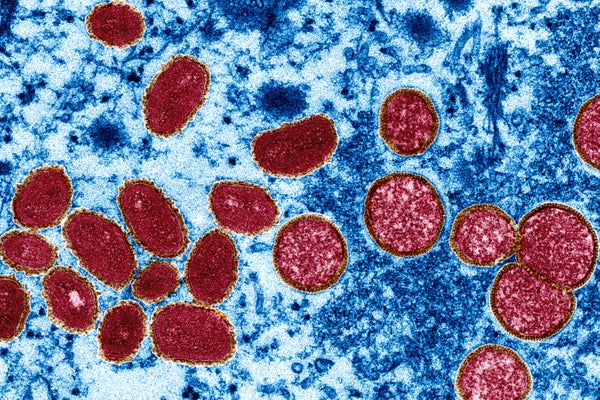
It’s been three weeks since public-health authorities confirmed a case of monkeypox in the United Kingdom. Since then, more than 400 confirmed or suspected cases have emerged in at least 20 non-African nations, including Canada, Portugal, Spain and the United Kingdom — the largest outbreak ever seen outside Africa. The situation has scientists on alert, because the monkeypox virus has emerged in separate populations across multiple countries, and there is no obvious link between many of the clusters, raising the possibility of undetected local transmission of the virus.
“We need to act quickly and decisively, but there is still a lot to be learned,” says Anne Rimoin, an epidemiologist at the University of California, Los Angeles, who has studied monkeypox in the Democratic Republic of the Congo for more than a decade.
Nature outlines some of the key questions about the recent outbreaks that researchers are racing to answer.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
How did the current outbreaks start?
Since the latest outbreaks began, researchers have sequenced viral genomes collected from people with monkeypox in countries including Belgium, France, Germany, Portugal and the United States. The most important insight they have gained so far is that each of the sequences closely resembles that of a monkeypox strain found in West Africa. The strain has a death rate of less than 1% in poor, rural populations, making it much less lethal than another that has been detected in Central Africa. That one has a fatality rate of up to 10%.
Clues have also emerged about how the outbreak might have begun. Although researchers need more data to confirm their suspicions, the sequences they have evaluated so far are nearly identical, suggesting that a thorough epidemiological investigation might find that the recent outbreaks outside Africa all link back to a single case.
The current sequences are most similar to those from a smattering of monkeypox cases that arose outside Africa in 2018 and 2019 that were linked to travel in West Africa. The simplest explanation is that the person who had the first non-African case this year — who has still not been identified — became infected through contact with an animal or human carrying the virus while visiting a similar part of Africa, says Bernie Moss, a virologist at the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland.
But other explanations cannot be ruled out, says Gustavo Palacios, a virologist at the Icahn School of Medicine at Mount Sinai in New York City. It’s possible that the virus was already circulating, undetected, outside Africa in humans or animals, having been introduced during earlier outbreaks. This hypothesis, however, is less likely because monkeypox usually causes visible lesions on people’s bodies — which would probably be brought to the attention of a physician.
Could a genetic change in the virus explain the latest outbreaks?
Understanding whether there is a genetic basis for the virus’s unprecedented spread outside Africa will be incredibly difficult, says Elliot Lefkowitz, a computational virologist at the University of Alabama at Birmingham who has studied poxvirus evolution. Researchers are still struggling to determine precisely which genes are responsible for the higher virulence and transmissibility of the Central African strain compared with the West African one more than 17 years after they identified a difference between the two.
One reason for this is that poxvirus genomes contain many mysteries, Lefkowitz says. The monkeypox genome is enormous relative to that of many other viruses — it is more than six times as large as the genome for the SARS-CoV-2 coronavirus. That means monkeypox genomes are at least “six times harder to analyse”, says Rachel Roper, a virologist at East Carolina University in Greenville, North Carolina.
Another reason, Palacios says, is that few resources have been dedicated to genomic-surveillance efforts in Africa, where monkeypox has been a public-health concern for many years. So virologists are in the dark, because they have few sequences to which they can compare the new monkeypox sequences, he says. Funding agencies have not heeded scientists, who have been warning for more than a decade1 that further monkeypox outbreaks could occur, he adds.
Ifedayo Adetifa, the head of the Nigeria Centre for Disease Control in Abuja, says that African virologists he’s spoken to have expressed irritation that they’ve struggled to garner funding and publish studies about monkeypox for years — but that now it’s spread outside the continent, public-health authorities worldwide suddenly seem interested.
To understand how the virus evolves, it would also be useful to sequence the virus in animals, Palacios says. The virus is known to infect animals — mainly rodents such as squirrels and rats — but scientists have yet to discover its natural animal reservoir in the affected areas of Africa.
Can the outbreaks be contained?
Understanding whether there is a genetic basis for the virus’s unprecedented spread outside Africa will be incredibly difficult, says Elliot Lefkowitz, a computational virologist at the University of Alabama at Birmingham who has studied poxvirus evolution. Researchers are still struggling to determine precisely which genes are responsible for the higher virulence and transmissibility of the Central African strain compared with the West African one more than 17 years after they identified a difference between the two.
If deployed, the vaccines would probably be used in a ‘ring vaccination’ strategy, which would inoculate close contacts of infected people. Andrea McCollum, an epidemiologist who heads the poxvirus team at the CDC, says that the agency is not yet deploying such a strategy. But CNN reports that the United States plans to offer smallpox vaccines to some health-care workers treating infected people. It might also be worth considering vaccinating groups at a higher risk of infection, in addition to close contacts of infected people, Rimoin says.
Even if public-health officials can halt the transmission of monkeypox in humans during the current outbreaks, virologists are concerned that the virus could spill back into animals. Having new reservoirs of virus in animals would increase the probability of it being transmitted to people again and again, in countries including those that don’t have any known animal reservoirs of the virus. On 23 May, the European Centre for Disease Prevention and Control highlighted this possibility, but deemed the probability “very low”. Nevertheless, European health officials strongly recommended that pet rodents such as hamsters and guinea pigs belonging to people with confirmed cases of monkeypox be either isolated and monitored in government facilities or, as a last resort, euthanized, to avoid the possibility of spillover.
Although the risk is low, Moss says the main concern is that scientists wouldn’t know if such a spillover event occurred until it was too late, because infected animals typically don’t show the same visible symptoms seen in humans.
Is the virus spreading differently compared with previous outbreaks?
Monkeypox virus is known to spread through close contact with the lesions, bodily fluids and respiratory droplets of infected people or animals. But health officials have been examining sexual activity at two raves in Spain and Belgium as drivers of monkeypox transmission, according to the Associated Press, raising speculation that the virus has evolved to become more adept at sexual transmission.
The linking of cases to sexual activity doesn’t mean that the virus is more contagious or is transmitted sexually, however — just that the virus spreads readily through close contact, Rimoin says. Unlike SARS-CoV-2, which isn’t thought to linger on surfaces much, poxviruses can survive for a long time outside the body, making surfaces such as bedsheets and doorknobs potential vectors of transmission, Roper says.
Although health officials have noted that many cases have been among men who have sex with men (MSM), Rimoin emphasizes that the most likely explanation for the virus’s spread among MSM groups is that the virus was coincidentally introduced into the community, and it has continued spreading there.
All of the new attention on monkeypox has laid bare just how much scientists have yet to understand about the virus, McCollum says. “When this has all settled down, I think we’ll have to think long and hard about where the research priorities are,” she says.
This article is reproduced with permission and was first published on May 27 2022.